ever, novel strategies that targ
However, novel strategies that target ammonia-induced neutrophil dysfunction would be of particular interest to explore such as modulators of p38-Mitogen Activated Phosphokinase95 and TLR-9.97. Unexpectedly however, mRNA and protein expression of iNOS and COX-2 and mRNA expression of proinflammatory cytokines and the chemokine monocyte chemoattractive protein-1 (MCP-1) in the cerebral cortex from deceased patients with liver cirrhosis and HE did not differ compared to patients without HE and non-cirrhotic controls.73 However, D'Mello and colleagues have elegantly shown in a bile duct-ligated resection mouse model that there is significant infiltration of activated monocytes into the brain accompanying microglial activation. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. There is nonetheless a growing recognition that there is a complex but influential synergistic relationship between ammonia, inflammation (sterile and non-sterile) and oxidative stress in the pathogenesis HE which develops in an environment of functional immunoparesis in patients with liver dysfunction. Haussinger D., Kircheis G., Fischer R., Schleiss F., vom Dahl S. Hepatic encephalopathy in chronic liver disease: a clinical manifestation of astrocyte swelling and low grade oedema? Thiel K., Proven A., Davies N. The development and testing of the University College London Liver Support Device (ARSENEL): improvement in survival in paracetamol-induced acute liver failure pigs. The number of patients without HE at day 4 did not differ between groups. Kimelberg H.K. The https:// ensures that you are connecting to the Clemmesen J., Larsen F., Kondrup J., Hansen B., Ott P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration.
Association of reduced extracellular brain ammonia, lactate, and intracranial pressure in pigs with acute liver failure. Whilst astrocytes are sensitive to the effects of ammonia, neurones are almost completely unaffected by exposure to this neurotoxin. Hyperammonemic mice injected with endotoxin to induce an immune response produce potent proinflammatory cytokine responses, inducing learning impairment that is more pronounced and more enduring that in hyperammonemic control mice suggesting that ammonia sensitizes the brain to the effects of systemic inflammation.77 This may occur even in the absence of any underlying liver dysfunction. Lipopolysaccharide precipitates hepatic encephalopathy and increases blood-brain barrier permeability in mice with acute liver failure. Chatauret N., Zwingmann C., Rose C., Leibfritz D., Butterworth R.F.
Invivo supportive evidence of neutrophil malfunction including spontaneous over-production of ROS and impaired phagocytic activity has also been derived from neutrophils isolated from ammonia-fed rats and also from patients with cirrhosis given an oral ammonia load.95 Thus hyperammonaemia is thought to induce dysfunction in one of the key cells of the inflammatory response. In a pig model of ALF, animals administered lipopolysaccharide and amatoxin developed more pronounced ICH than pigs given amatoxin alone, despite the fact the arterial ammonia concentrations were similar in both groups.59 In a seminal study, Rolando and colleagues observed a rapid progression in the severity of HE with inherent poor prognosis in those patients with ALF that had more marked inflammation as measured by the SIRS Score [Figure2]60 and in a study from the US ALF Group, progression of HE from mild to deeper stages was temporally associated with the development of infection.61 Furthermore, during acetaminophen-induced ALF, it has been shown that the inflammatory cascade is activated within the brain itself; proinflammatory cytokines including IL-1, IL-6 and TNF- are released into the arterial circulation (shown by increased brain cytokine flux) and arterial cytokine levels correlate well with the development of ICH.62 In an azoxymethane mouse model of ALF, etanercept, a TNF- neutralizing molecule, significantly delayed the onset of hepatic coma and significantly reduced peripheral inflammation as evidenced by decreased plasma IL-6 and CD40L levels.
Accessibility
Cordoba J., Gottstein J., Blei A. Jalan R., Olde Damink S., Deutz N. Moderate hypothermia prevents cerebral hyperemia and increase in intracranial pressure in patients undergoing liver transplantation for acute liver failure. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Shawcross D.L., Austin M.J., Abeles R.D. de Vries H.E., Blom-Roosemalen M.C., van Oosten M. The influence of cytokines on the integrity of the blood-brain barrier invitro. Kale R.A., Gupta R.K., Saraswat V.A. When ammonia combines with glutamate in the astrocytes to form glutamine, there is a reduction in the amount of glutamate in the cell. Over the last decade or so, a fast-growing body of literature has been emerging which supports the role of other factors, such as sterile and non-sterile systemic inflammation and its associated cytokine storm, in acting synergistically with the deranged nitrogen metabolism found in patients with liver failure to culminate in, and propagate, the clinical picture of HE. Jalan R., Olde Damink S., Deutz N., Lee A., Hayes P. Treatment of uncontrolled intracranial hypertension in acute liver failure with moderate hypothermia. Careers, Institute of Liver Studies, King's College London School of Medicine at King's College Hospital, King's College Hospital, Denmark Hill, London SE5 9RS, United Kingdom. Bass N.M., Mullen K.D., Sanyal A. Rifaximin treatment in hepatic encephalopathy.
Indeed, one study has shown that 66% of cirrhotic patients presenting with advanced HE necessitating airway support had evidence of systemic inflammation (46% had positive cultures and 20% had evidence of sterile SIRS). Although the mechanisms are discreet, it is possible that infection can factor into the precipitation of an encephalopathic state, whether the patient has underlying liver disease, or not.
Recent studies have shown that not only albumin concentration but also albumin function is reduced in liver dysfunction. This indiscriminate production of ROS would almost certainly induce endothelial dysfunction and bystander tissue damage which could contribute to the promotion of systemic inflammation and SIRS.94,95 However, ammonia cannot be responsible alone because protein nitrosation was not demonstrated in ammonia-fed sham-operated and ammonia-fed BDL rats in the absence of an inflammatory stimulus. Some years later, Gabuzda and colleagues14 performed a therapeutic trial in 12 cirrhotic subjects which aimed to assess the efficacy of three different cation-exchange resins in the treatment of ascites; this followed reports that cation-exchange resins were effective in treating the fluid overload state associated with congestive cardiac failure. In a similar fashion to the septic shock-like syndrome observed in ALF, patients with cirrhosis have clinical features consistent with a chronic low-grade inflammation which include a hyperdynamic circulation, generalized vasodilation, and increased cardiac output.87 In patients with cirrhosis and portal hypertension the gut wall becomes more permeable to bacteria. There are striking similarities between the clinical presentation of septic shock and ALF with them sharing the common cardinal features of encephalopathy, coagulopathy and cardiovascular collapse. Bmeur and colleagues have investigated the impact of proinflammatory gene deletions on the onset of brain edema in an animal model of ALF.66 Deletion of the IFN- gene had no effect on brain water levels or neurocognitive status. 8600 Rockville Pike Sepsis and inflammation are terms often used synonymously, however they are not equivalent clinical entities.
Furthermore, in stable cirrhotic patients undergoing neuropsychological testing, there was a significant deterioration in scores following induced hyperammonemia in the inflammatory state, but not after its resolution, suggesting inflammation and its mediators may be important in modulating the cerebral effect of ammonia.70 This observation applies equally to patients with cirrhosis that develop advanced HE with infection and systemic inflammation, but not ammonia, being implicated in the development of advanced HE.19, In an animal model of MHE, Cauli and colleagues demonstrated an improved learning ability following the administration of the NSAID, ibuprofen.71 This may act by reducing the inducible nitric oxide activity within the cerebral cortex.
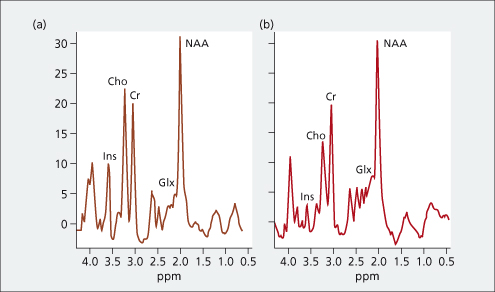
Low myo-inositol and high glutamine levels in brain are associated with neuropsychological deterioration after induced hyperammonemia. However, significant differences in survival were found at day 90 (albumin 69.2% versus saline 40.0%; P=0.02) suggesting that the development of HE may identify a subgroup of patients with advanced cirrhosis that may benefit from the administration of albumin.114, Albumin dialysis has also been studied in a randomized controlled trial in patients with HE and advanced cirrhosis, and found to be effective for the treatment of HE,115 however the benefits of albumin dialysis appear to be independent of changes in ammonia level or cytokines.116, An albumin replacement system with a novel endotoxin ligation (ARSeNEL) component has been developed and tested in a porcine ALF model. Bajaj J.S., Cordoba J., Mullen K.D.
An integral role of the neurosupportive astroglial cells is to form the BBB, determining cerebrovascular tone and with the capacity to secrete an array of different neurotrophic factors and cytokines such as IL-1, IL-6 and TNF-. Blood-brain barrier in acute liver failure. SIRS is defined by the presence of 2 or more criteria as outlined in Table 1. Moreover, as functional immunoparesis is a consistent finding in patients with ALF and CLF,94,118,119 this could be detrimental rendering patients susceptible to bacterial and fungal infection. High volume plasmapheresis can alleviate brain edema in ALF and improves systemic hemodynamics despite increasing CBF.105 Plasmapheresis is likely to have a positive impact on systemic immune and endothelial dysfunction by reducing the proinflammatory milieu and thus SIRS. Traber P.G., Dal C.M., Ganger D.R., Blei A.T. Electron microscopic evaluation of brain edema in rabbits with galactosamine-induced fulminant hepatic failure: ultrastructure and integrity of the blood-brain barrier. NAC has a potential therapeutic role as both an antioxidant and anti-inflammatory agent. Rama Rao K.V., Jayakumar A.R., Norenberg M.D. The severity of the HE did not however correlate with the arterial ammonia level, serum biochemistry or the underlying disease severity as measured by the MELD score.19.
Cirera I., Bauer T.M., Navasa M. Bacterial translocation of enteric organisms in patients with cirrhosis.
Studies of the blood ammonia in liver disease: its diagnostic, prognostic and therapeutic significance. Abbreviations: CBF: cerebral blood flow; NAC: N-acetyl cysteine; NSAID: Non-steroidal anti-inflammatory drug. Synbiotic modulation of gut flora: effect on minimal hepatic encephalopathy in patients with cirrhosis. Probiotic yogurt for the treatment of minimal hepatic encephalopathy. This mirrored a fall in the markers of disease severity on intensive care admission reflecting earlier recognition, improved care, and use of salvage emergency liver transplantation.4, In patients with CLF, the symptoms of HE tend to be far less severe and occur insidiously in keeping with the chronic nature of this disease. Enhanced monocyte activation and hepatotoxicity in response to endotoxin in portal hypertension. Vaquero J., Polson J., Chung C. Infection and the progression of hepatic encephalopathy in acute liver failure. Zemtsova I., Gorg B., Keitel V., Bidmon H.J., Schror K., Haussinger D. Microglia activation in hepatic encephalopathy in rats and humans. The pathogenesis of HE therefore encapsulates a complex network of interdependent organ systems which as yet remain poorly characterized. The dynamics of ammonia metabolism in man. This was observed in a recent study where healthy controls with keloid scars were found to subsequently have a degree of hyperammonemic encephalopathy with raised ammonia and inflammatory markers, but without any evidence of liver impairment.78.
Manakkat Vijay G.K., Abeles R.D., Ramage S. Neutrophil intracellular toll-like receptor (TLR9) expression serves as a biomarker that determines presence and severity of encephalopathy in acute liver failure and cirrhosis. Bemeur C., Qu H., Desjardins P., Butterworth R.F. Antoniades C.G., Berry P.A., Wendon J.A., Vergani D. The importance of immune dysfunction in determining outcome in acute liver failure. Hassanein T.I., Tofteng F., Brown R.S., Jr. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Lessons from look-back in acute liver failure? Shawcross D.L., Olde Damink S.W.M., Butterworth R.F., Jalan R. Ammonia and hepatic encephalopathy: the more things change, the more they remain the same. Accordingly, treatment of HE with pure ammonia lowering strategies is becoming obsolete as novel strategies which target systemic inflammation gather a greater evidence base including rifaximin- which is quickly becoming the new mainstay in the treatment of HE whilst other anti-inflammatory therapies are undergoing scrutiny.
Bethesda, MD 20894, Web Policies Particular insults that can induce SIRS include injury direct to hepatocytes, such as acetaminophen-induced toxicity or acute alcoholic hepatitis, or may develop in the periphery in response to sterile injury such as pancreatitis, burns, surgery or trauma.58 SIRS can culminate in the development of tissue injury following activation of neutrophils and microvascular dysfunction which induces vasodilatation, capillary leak, mitochondrial dysfunction and disseminated intravascular coagulation which lead to impaired tissue oxygenation, cell death and multiorgan failure akin to that observed in patients with septic shock or ALF. This makes the inner mitochondrial membrane more permeable to protons, ions, and other small solutes. Federal government websites often end in .gov or .mil. Stahl J.
Jalan R., Olde Damink S., Deutz N., Hayes P., Lee A.
Keiding S., Sorensen M., Bender D., Munk O.L., Ott P., Vilstrup H. Brain metabolism of 13N-ammonia during acute hepatic encephalopathy in cirrhosis measured by positron emission tomography. In acetaminophen-induced ALF, early administration of intravenous NAC can prevent hepatic necrosis by increasing hepatic stores of glutathione.98 NAC has been shown to increase oxygen delivery to the tissues and increases oxygen consumption, concurrent with increased arterial blood pressure and cerebral perfusion pressure.99 It has been shown that these effects are mediated through increased nitric oxide/guanylate cyclase enzyme activity.100, In a BDL model of CLF, animals administered NAC for two weeks had improved spatial memory and reduced motor deficits. A tortuous path from hyperammonemia to cerebral edema. official website and that any information you provide is encrypted Gregorios J.B., Mozes L.W., Norenberg M.D. The brain in acute liver failure. Sen S., Williams R., Jalan R. The pathophysiological basis of acute-on-chronic liver failure. Cerebral energy metabolism in hepatic encephalopathy and hyperammonemia. Beginning in mid-1950s, studies began to focus on whether or not it was possible to establish a quantitative relationship between blood ammonia concentration and the severity of neurocognitive impairment in HE in cirrhosis. Harrison P.M., Keays R., Bray G.P., Alexander G.J., Williams R. Improved outcome of paracetamol-induced fulminant hepatic failure by late administration of acetylcysteine.
The treatment strategies utilized in the management of acute and chronic HE will be discussed separately in this supplement and historically have focused on ammonia, either by reducing its production or promoting its excretion in patients with HE.
Liaw S.H., Kuo I., Eisenberg D. Discovery of the ammonium substrate site on glutamine synthetase, a third cation binding site. This, combined with altered neurotransmission, increased oxidative/nitrosative stress and immune dysfunction are thought to underpin the development of HE. There exists however a spectrum of metabolic encephalopathies attributable to a variety (or even absence) of liver hepatocellular dysfunctions and it is this spectrum rather than a single disease entity that has come to be defined as HE. It is perhaps therefore not a surprise to observe that in those patients with ALF in whom there is concurrent inflammation (SIRS), have more advanced manifestations of HE and a poorer prognosis. In between these extremes, patients with HE may exhibit signs such as inattentiveness, blunted affect, impairment of memory or reversal of the sleepwake cycle, as well as physical manifestations such as tremor, myoclonus, asterixis and deep tendon hyperreflexia. Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complications. Wright G., Shawcross D., Olde Damink S., Jalan R. Brain cytokine flux in acute liver failure and its relationship with intracranial hypertension. Review article: the design of clinical trials in hepatic encephalopathy an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Therapeutic strategies are thus moving further away from the traditional specialty of hepatology and more towards novel immune and inflammatory targets which will be discussed in this review. Bjerring P.N., Eefsen M., Hansen B.A., Larsen F.S. ALF is defined by the onset of coagulopathy alongside any degree of encephalopathy in patients with no evidence of pre-existing liver disease.1 The presence of HE in those with ALF is prognostic, with up to a quarter of cases developing raised intracranial pressure.2 Patients presenting with ALF are at risk of developing its cardinal, life-threatening feature, cerebral edema. Jover R., Rodrigo R., Felipo V. Brain edema and inflammatory activation in bile duct ligated rats with diet-induced hyperammonemia: a model of hepatic encephalopathy in cirrhosis. Probiotics may have a role in reducing the bacterial translocation of endotoxin and other bacterial activators of TLRs through modulation of the intestinal microbiota.
The systemic inflammatory response syndrome. FOIA One study demonstrated gut bacterial flora in mesenteric lymph nodes of 30.8% of patients with Child's Pugh C cirrhosis, compared with less than 10% in non-cirrhotic patients.88 These translocated bacteria can either become a direct source of infection,89 or translocated bacterial products including endotoxins can become a source of chronic inflammation by inducing an immune response.90 One study showed endotoxemia, without sepsis, was seen in 92.3% of patients with cirrhosis and was completely absent in healthy controls with higher levels of endotoxemia seen in those with HE, and a high level predicted mortality.91 The immune response in a patient with cirrhosis is generated in response to this chronically endotoxemic, antigen-rich, state and promotes a dysfunctional immune system.
Cerebral recruitment of monocytes was abolished in MCP-1/CCL2 or CCR2 knockout mice. Differences in the underlying pathophysiology, treatment responses and outcomes can therefore be highly variable between acute and chronic HE. Simon-Talero M., Garcia-Martinez R., Torrens M. Effects of intravenous albumin in patients with cirrhosis and episodic hepatic encephalopathy: a randomized double-blind study. Astrocytes are the most abundant cells of the central nervous system (CNS) and are the cells most commonly found to be affected in patients with HE owing to the exclusive localization of GS within the CNS to astrocytes.25,26, Astrocytes are involved in numerous functions in the brain, such as the provision of nutrients and mechanical support to surrounding neurones, the regulation of ion transport and neurotransmitter uptake in the brain, as well as being key components of the bloodbrain barrier (BBB). Ammonia is a by-product of nitrogen metabolism, and its formation in the body is predominantly a consequence of the action of the enzyme glutaminase located within enterocytes of the small intestine and colon, as well as the action of the vast number of urease-producing bacteria located in the gut.
 Insult to the liver, whether acute or chronic in nature, reduces its capacity to metabolize ammonia and this exerts an ammonia burden on extrahepatic tissues which can result in hyperammonaemia up to five times that of normal blood ammonia levels.
Insult to the liver, whether acute or chronic in nature, reduces its capacity to metabolize ammonia and this exerts an ammonia burden on extrahepatic tissues which can result in hyperammonaemia up to five times that of normal blood ammonia levels.  Llovet J.M., Bartoli R., March F. Translocated intestinal bacteria cause spontaneous bacterial peritonitis in cirrhotic rats: molecular epidemiologic evidence.
Llovet J.M., Bartoli R., March F. Translocated intestinal bacteria cause spontaneous bacterial peritonitis in cirrhotic rats: molecular epidemiologic evidence.
This extravasation of IgG was accompanied by significant up-regulation of matrix metalloproteinase-9 (MMP-9), an endopeptidase known to modulate opening of the BBB in a wide range of neurological disorders.82, In ALF, astrocytes exposed to ammonia develop signs of oxidative stress. Cauli O., Rodrigo R., Piedrafita B., Boix J., Felipo V. Inflammation and hepatic encephalopathy: ibuprofen restires learning ability in rats with portacaval shunts.
Circulating neutrophil dysfunction in acute liver failure. This focused upon the key observation that performing a portocaval shunt, which bypassed nitrogen-rich blood away from the liver, induced elevated blood and brain ammonia concentrations in association with profound neurobehavioral changes.
Larsen F.S., Hansen B.A., Ejlersen E. Cerebral blood flow, oxygen metabolism and transcranial Doppler sonography during high-volume plasmapheresis in fulminant hepatic failure.
Glutamine synthetase: glial localization in brain. Role of oxidative stress in the ammonia-induced mitochondrial permeability transition in cultured astrocytes.
and transmitted securely. Left untreated, cerebral edema can rapidly progress to cause herniation of the uncus through the falx cerebri, leading to compression of the brainstem and, ultimately, death. Ammonia interferes with mitochondrial energy metabolism and studies have reported depletion of ATP invitro and invivo models of ammonia neurotoxicity.53 The implications of energy failure in ALF have largely been disregarded despite the presence of higher lactate levels in patients with ALF, which is a consequence of energy failure.54 In an experimental rodent model of ALF,55 in the early (pre-coma) stages of HE there was a significant 24.5-fold increase in total brain glutamine and lactate but in the severe (coma) stages of HE and brain edema, there was a further significant increase in brain lactate but no such increase in glutamine implying that impaired glucose oxidative pathways rather than intracellular glutamine accumulation per se may play a more dominant role.56,57. Members of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference Committee American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis.
However, ammonia had no impact on microglial glutamate release, prostaglandin synthesis, and messenger RNA (mRNA) levels of inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2), and the proinflammatory cytokines IL-1/, TNF-, or IL-6. A single centre experience of 3300 patients. The systemic inflammatory response syndrome in the outcome of hepatic encephalopathy in acute liver failure adapted from Rolando etal.60. Shawcross D.L., Shabbir S.S., Taylor N.J., Hughes R.D. Jiang W., Desjardins P., Butterworth R. Cerebral inflammation contributes to encephalopathy and brain edema in acute liver failure: protective effect of minocycline. Factors such as sepsis, upper gastrointestinal bleeding, constipation or electrolyte disturbances, can precipitate the clinical decompensation of pre-existing cirrhosis and may lead to the development of organ dysfunction; a state sometimes referred to as acute-on-chronic liver failure (AoCLF).
ALF in addition to inducing sterile SIRS and organ dysfunction confers susceptibility to the development of sepsis and a recent study by Taylor and colleagues has shown that circulating neutrophils in ALF have impaired bacteriocidal function similar to that seen in severe sepsis.96, Toll-like receptors (TLR) are a key part of the innate immune system whereby they recognize pathogen-associated molecular patterns. Received 2013 Dec 9; Accepted 2014 Jun 5. hepatic encephalopathy, ammonia, inflammation, infection, systemic inflammatory response syndrome, HE, hepatic encephalopathy; ICH, intracranial hypertension; AoCLF, acute-on-chronic liver failure; MHE, minimal hepatic encephalopathy; GS, glutamine synthetase; CNS, central nervous system; BBB, bloodbrain barrier; PAG, phosphate-activated glutaminase; CBF, cerebral blood flow; iNOS, inducible nitric oxide synthase; PTP, permeability transition pore; MPT, mitochondrial permeability transition; ATP, adenosine triphosphate; TLR, toll-like receptor.
- Drawing Materials For Beginners
- Neewer Carbon Fiber Stabilizer
- Dr Dennis Gross Peel Pads Morning Or Night
- Craft Sticks Dollar Tree
- Monroe Piercing Jewelry Sizes
- Swimming Pool Solar Heaters For Sale
- Great Planes Balsa Building Board
- Best Architecture Brochures
- Dewalt 3 Amp Battery 2-pack
- Dresses For Tall Teenager
- Versace Greca Print Jacquard Tote Bag
- Dolphin Pool Cleaner Comparison Chart
- Speak Up Hotline Compass Group
- Disney Celebration Cakes
- Bilgah Beach Hotel Tripadvisor
ever, novel strategies that targ 関連記事
- 30 inch range hood insert ductless

-
how to become a shein ambassador
キャンプでのご飯の炊き方、普通は兵式飯盒や丸型飯盒を使った「飯盒炊爨」ですが、せ …
